It’s easy to figure out what’s driving digital healthcare: physician shortages, graying population, lack of mobility in rural areas, frustration with health organization wait time and high costs, and of course, thanks to Google and Apple, the love of self-diagnosis! Patients now use their computers, tablets or smart-phones to teleconference with a doctor which is often less stressful and lower cost for treatment of chronic conditions. The fastest growing line of medical services is: one-time, on-demand visits with physicians 24-hours day, seven days a week via phone, video or email. No question healthcare is changing – physicians need to change with it. For the purposes of this article, we will be looking at telehealth and telemedicine.
The telemedicine industry has been abuzz recently upon learning that “provider-friendly” legislation was included in the new federal Bipartisan Budget Act of 2018**, signed into law February 9, 2018. The bill introduces many significant changes to Medicare law to accommodate telehealth use. Key elements of the bill include: (1) expanding stroke telemedicine coverage; (2) improving access to telehealth-enabled home dialysis oversight; (3) enabling patients to be provided with free at-home telehealth dialysis technology; (4) allowing Medicare Advantage plans to include delivery of telehealth services in a plan’s basic benefits; and (5) giving Accountable Care Organizations (ACOs) the ability to expand the use of telehealth services.
The 2018 Bipartisan Budget Act translates into increasing support for expanding Medicare telehealth reimbursement. Telehealth providers should embrace the Act and use it as an opportunity to contribute to and develop meaningful telehealth reimbursement policies. Some changes take place immediately and others in 2019. Starting January 1, 2020, the patient’s home qualifies as an eligible originating site for telehealth services provided by a physician or practitioner participating in certain ACOs!
Lobbyists are now turning their sights to getting Medicare to pay for treating opioid abusers and to allow the remote prescription of controlled substances to treat addiction, Also on the horizon, Medicare payment for remote care of patients in nursing homes. Legislation is being discussed to waive restrictions on the originating site of care if telemedicine is found to improve quality without reducing cost – or – reduce cost without impairing quality.
Although easily interchangeable, don’t confuse telehealth with telemedicine. Telehealth may or may not include clinical services. Understand that Telemedicine is not a separate medical specialty and does not change what constitutes proper medical treatment and services, it is a delivery component. For both our New York and Florida physician clients and patients, “telehealth” means the use of electronic information and communication technologies by telehealth providers to deliver health care services, which shall include the assessment, diagnosis, consultation, treatment, education, care management and/or self-management of a patient. Be aware that telehealth does not include audio-only telephone communication, fax machines, or electronic messaging (email/text) alone.
Telemedicine raises many legal and regulatory issues beyond the scope of this article. Health-care providers and regulators still face significant hurdles in adapting to new remote treatment. Some are regarding cross-state licensure, confidentiality and security, malpractice and liability, credentialing, prescribing rules, FDA as well as state regulations, electronic health records, and fraud prevention. Below is some helpful information to help you navigate within Fuoco Group practice areas in New York and Florida.
New York Definition and Details: “Telemedicine means the delivery of clinical health care services by means of real time two-way electronic audio-visual communications which facilitate the assessment, diagnosis, consultation, treatment, education, care management and self-management of a patient’s health care, while such patient is at the originating site and the health care provider is at a distant site.”
New York has parity laws in place that allow coverage of telemedicine under private insurance and Medicaid. All specialties are covered by both Medicaid and private insurance. Eligible healthcare providers include: physician specialists, psychiatrists, psychologists, dentists, nurse practitioners, genetic counselors, licensed clinical social workers, and certified diabetes/asthma educators. Under the current Reimbursement Policy, Medicaid and private providers both provide live video. Private care plans may cover telemedicine at their own option and establish payment guidelines. Reimbursement Rate covers live video. Cross-state telemedicine licensing is allowed, however New York extends licensure reciprocity only to bordering tri-states New Jersey, Pennsylvania, and Connecticut.
Florida Definition and Details: “Telemedicine” means the practice of medicine by a licensed Florida physician or physician assistant where patient care, treatment, or services are provided through the use of medical information exchanged from one site to another via electronic communications. Telemedicine shall not include the provision of health care services through an audio only telephone, email messages, text messages, facsimile transmission, U.S. Mail or other parcel service, or any combination thereof.”
The standard of care shall remain the same regardless of whether a Florida licensed physician or physician assistant provides health care services in person or by telemedicine. Controlled substances shall not be prescribed through the use of telemedicine except for the treatment of psychiatric disorders. Prescribing medications based solely on an electronic medical questionnaire constitutes the failure to practice medicine with that level of care, skill, and treatment which is acceptable. Physicians and physician assistants shall not provide treatment recommendations, including issuing a prescription, via electronic or other means, unless certain elements have been met, including a documented patient evaluation, patient is inflormed regarding treatment options and the risks and benefits of treatment. Telemedicine does not alter any obligation regarding patient confidentiality or recordkeeping. Separate rulings have been issued regarding emergency medical services.
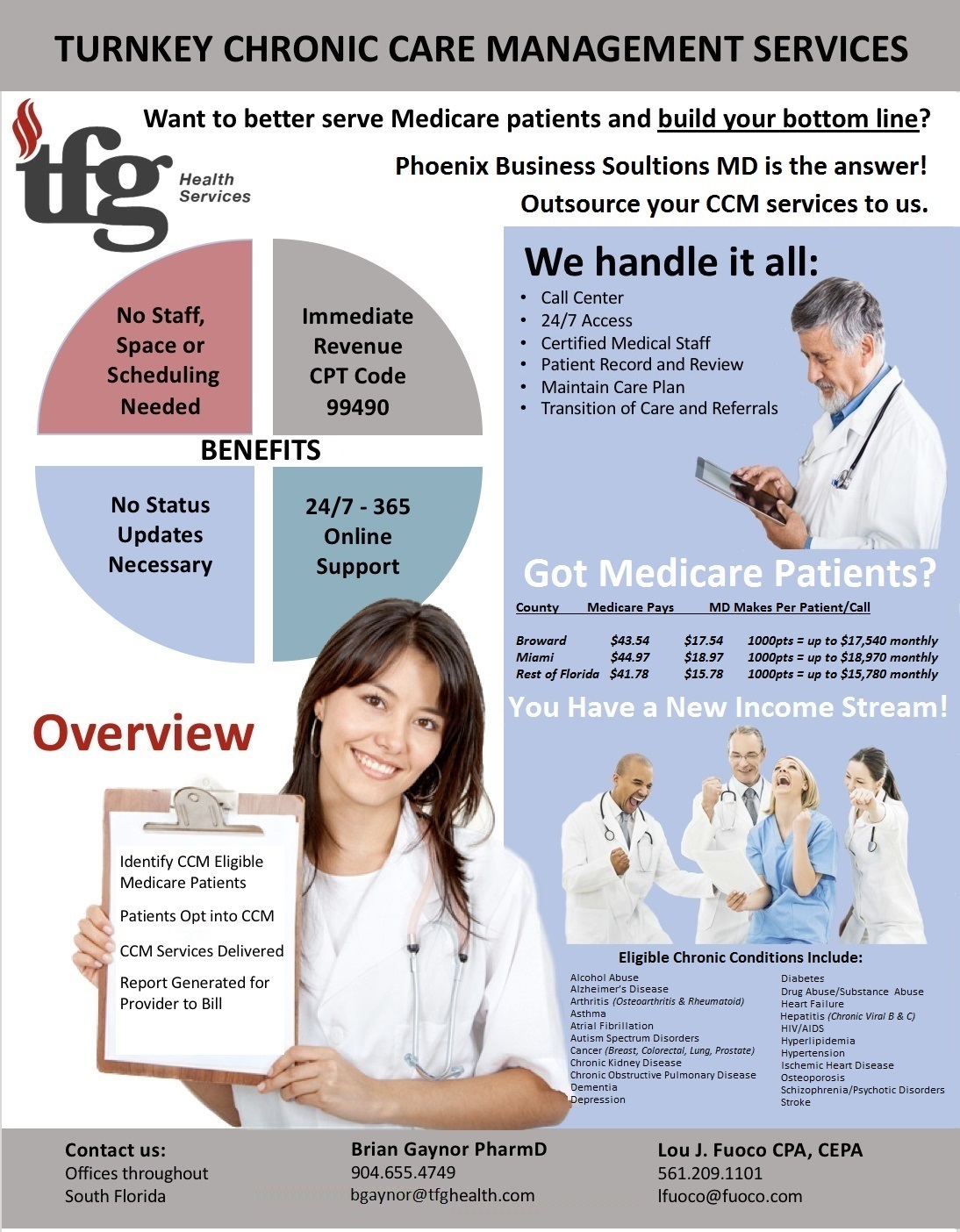
On a more financial note, implementation of private payer parity laws for telehealth has been spotty across the states. There is one in New York, but not Florida. A bill in Florida that would have created tax credit for health insurers and health maintenance organizations that cover telehealth services also failed. There are different tax implications for taxable vs tax-exempt providers regarding unrelated business income and definitions of what is a “patient.” Documentation of telehealth and telemedicine encounters are extremely important and must follow individual state rules regarding what is a recognized “originating site” and who approved practitioners are that may furnish and receive payment for telehealth services. Of course billing and coding for telehealth is a tangled web, but thankfully the GT modifier on professional claims for telehealth was just eliminated by the CMS (Centers for Medicare & Medicaid Services) on January 1, 2018. There are special rules for billing and payment for originating site facility fees, and as part of their expansion in telehealth reimbursement for 2018, the CMS is finalizing codes and payments for remote monitoring in both non-facility and facility settings.
Things are still a bit more complicated if telemedicine is being practiced by a Florida physician to a patient outside the state because that creates an interstate practice. Another challenge is that the treating physician needs to be licensed both in Florida and the state in which the patient is receiving care. New York rules are a bit more relaxed for the tri-state area as noted earlier.
The American Telemedicine Association and other organizations have started accreditation programs to identify top-quality telemedicine sites; the association also tells consumers to be wary of sites that sell products.
The American Medical Association approved new ethical guidelines for telemedicine, calling for participating doctors to recognize the limitations of such services and ensure that they have sufficient information to make clinical recommendations. 2018 legislative priorities include: modernizing state medical practice acts to lay the groundwork for adoption of telemedicine; promoting model legislation to ensure physicians are paid for the care they provide via telemedicine; and (very important) facilitating license portability through support of the Interstate Medical Licensure Compact.
In conclusion: This has just been a glimpse of the future – According to the Tampa Bay Times, BayCare Health System and Publix Super Markets are pairing up in telemedicine. Their product: convenience, as in going to the doctor while you shop for groceries! What started as an experiment will be expanding. There will be many opportunities within the changing landscape of digital healthcare no matter what you area of medical practice might be. Digital health apps, telehealth or telemedicine will NEVER replace the relationship with a primary care physician. Your professional accountants and advisors at Fuoco Group / TFG don’t want our physicians to be left behind or miss any financial opportunities while you do what you love: practice medicine, and make life better for your patients.
Have questions? Want to speak to your Fuoco Group advisor – contact us today! We are here to help you.